The How to Quit Smoking Guide: Why, How and Preferred Therapy

Tips For Every Woman Going Through Menopause
Table of Contents
Irritable bowel syndrome (IBS) affects about one in 20 American and about 1 in 10 people globally. Researchers know it is related to a disorder in the brain-gut connection, but they do not fully understand the causes of IBS. Usually thought to come from a unique combination of factors in each individual, its main symptoms are abdominal pain and bloating. Symptoms may come and go over a lifetime, or they may be severe and chronic. Learn which seven foods to avoid with IBS and how to improve the quality of your life with hypnosis for IBS.
Seven Food Groups To Avoid With IBS
Because IBS affects individuals differently, not everyone reacts to foods in the same way. The National Institute of Diabetes and Digestive and Kidney Diseases recommends a diet that is low in hard-to-digest carbohydrates. Other research recommends avoiding or limiting these seven foods that trigger IBS symptoms:
1. Alcohol
More study is needed, but a 2013 article in the American Journal of Gastroenterology suggested a link between heavy drinking and an increase in IBS symptoms. Researchers concluded that individual drinking patterns may determine the effect of alcohol on IBS. They also noted that alcohol can reduce the body’s ability to absorb and digest carbohydrates, worsening the effects of certain foods.
2. Caffeine
Like alcohol, the amount of caffeine consumed and the effect it has on the individual may determine its impact on IBS. Because caffeine may stimulate the intestines, it can also worsen diarrhea. A cup of coffee in the morning may be okay, but other products also contain caffeine. Check the content on carbonated beverages, chocolate, energy drinks, green tea and pain medication to make sure you are not consuming more than you think.
3. Insoluble Fiber
In the past, doctors recommended fiber to patients with IBS. While healthy fiber is necessary, you may not need as much as you think. The topic is still being debated, but studies show that fiber can increase bloating, abdominal pain, and distension. Current guidelines rely on several variables, including how long it takes fiber to ferment and how soluble it is in the intestines. Soluble fiber absorbs water, slows down digestion, and can cause constipation. It is found in nuts, seeds, beans, lentils, peas, oat bran, and specific fruits and vegetables. Psyllium, a dietary supplement, also contains soluble fiber.
4. Spicy Foods
Spicy foods trigger IBS symptoms, and the cause is probably capsaicin, an ingredient in red chili pepper. How often it is consumed and the types of foods it is paired with seem to play a role in the severity of symptoms. Capsaicin may actually help to balance good bacteria in the gut, and it has anti-inflammatory properties. Like other foods, the answer seems to be to consume spicy foods in moderation or eliminate them entirely, depending on individual reactions.
5. High-Fat Foods
Foods that are high in fat, especially fried or processed foods, worsen diarrhea and other symptoms of IBS. Because fat slows down the rate of digestion, it also makes it difficult for the colon to release gas, causing bloating. If high-fat foods cause your IBS to flare, eliminate one food at a time until you find the culprit. Always avoid highly processed and fried foods.
6. Carbonated Beverages
Not drinking enough fluids leads to dehydration, and that makes constipation worse. Everybody needs an adequate supply, but carbonated beverages are not a good choice. A better option is water and non-caffeinated beverages like herbal tea. Carbonated beverages, including seltzer water, carbonated juice, and soft drinks, should be used in moderation or not at all. Artificial sweeteners should be avoided.
7. Milk and Dairy
Dairy products and milk are foods to avoid with IBS. They contain lactose, which is an irritant for many people; and they are usually high in fat, complicating the issue even further. You can have a test for lactose intolerance or switch to milk substitutes, such as almond or soy milk. If you avoid dairy products completely, make sure you get enough calcium from other sources.
Hypnotherapy for IBS
Do you trust your gut feelings? Studies now show a connection between the gut and the brain, and leading hospitals are using gut-directed hypnotherapy as part of a multidisciplinary treatment for IBS.
In a 2020 study, researchers compared IBS patients who received traditional care with those who were given a combination of traditional care and gut-directed therapy, including hypnotherapy. Among participants who received traditional care, 63% reported relief of symptoms. Among those who received traditional care and gut-directed therapy, 83% of participants reported symptom relief.
The evidence to support the effectiveness of gut-directed hypnotherapy for the relief of IBS symptoms is so strong that the American College of Gastroenterologists added the practice to its clinical guidelines in 2021. Not only is gut-directed hypnotherapy effective, but sessions can be done in person, virtually, or via an IBS hypnotherapy app.
Find Relief With an IBS Hypnotherapy App
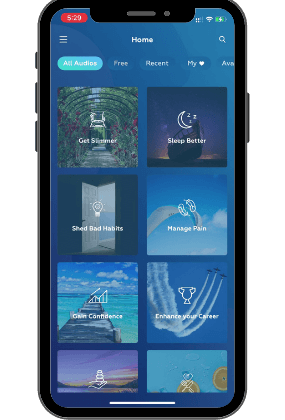
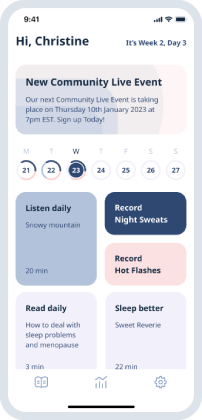
Self-hypnosis audios for IBS is an affordable, easy way to try gut-directed therapy. Get started with UpNow’s self hypnosis audios for IBS, or register for a monthly or annual plan. Enjoy access to self hypnosis downloads for IBS, anxiety, smoking cessation and other life-changing topics.
UpNow Health only uses high-quality sources, including peer-reviewed articles, to support the facts within our articles. All our articles are reviewed by experts to ensure that our content is accurate, helpful, and trustworthy.
1. Cozma-Petruţ, A., Loghin, F., Miere, D., & Dumitraşcu, D. L. (2017). Diet in irritable bowel syndrome: What to recommend, not what to forbid to patients!. World journal of gastroenterology, 23(21), 3771–3783. https://doi.org/10.3748/wjg.v23.i21.3771 Accessed 20th July 2022.
2. Reding, K. W., Cain, K. C., Jarrett, M. E., Eugenio, M. D., & Heitkemper, M. M. (2013). Relationship between patterns of alcohol consumption and gastrointestinal symptoms among patients with irritable bowel syndrome. The American journal of gastroenterology, 108(2), 270–276. https://doi.org/10.1038/ajg.2012.414 Accessed 20th July 2022.
3. Chamara Basnayake, Prof Michael A Kamm, Annalise Stanley, Amy Wilson-O’Brien, Kathryn Burrell, Isabella Lees-Trinca. Standard gastroenterologist versus multidisciplinary treatment for functional gastrointestinal disorders (MANTRA): an open-label, single-centre, randomised controlled trial. The Lancet, Gastroenterology & Hepatology. Volume 5, Issue 10, p890-899, October 01, 2020. https://doi.org/10.1016/S2468-1253(20)30215-6 Accessed 20th July 2022.
4. Lacy, Brian E. PhD, MD, FACG1; Pimentel, Mark MD, FACG2; Brenner, Darren M. MD, FACG3; Chey, William D. MD, FACG4; Keefer, Laurie A. PhD5; Long, Millie D. MDMPH, FACG (GRADE Methodologist)6; Moshiree, Baha MD, MSc, FACG7 ACG Clinical Guideline: Management of Irritable Bowel Syndrome, The American Journal of Gastroenterology: January 2021 – Volume 116 – Issue 1 – p 17-44. https://doi.org/10.14309/ajg.0000000000001036 Accessed 20th July 2022.