How Much Sleep Do We Need Each Night?

Transforming to a Growth Mindset with Self-Hypnosis
Table of Contents
Sleep is a complex biological process. When you sleep, your body releases neurotransmitters or chemical signals that help you fall asleep and stay asleep. Throughout the night, you will repeatedly cycle through various sleep stages. During the first stage, your muscles relax, and you may drift in and out of sleep or wake up easily. The second stage is a deeper stage during which your eye movement ceases and brain waves slow. The third stage of sleep is characterized by slow delta brain waves punctuated by faster brain waves, and the fourth stage consists of primarily delta waves.
The fifth and final stage of sleep is REM sleep. REM stands for “rapid eye movement,” and your eyes move rapidly. Your breathing may be irregular, and your blood pressure and heart rate increase. Your limbs are temporarily paralyzed during this stage of sleep. It typically takes a little more than an hour to reach REM sleep after you first fall asleep. Completing the entire cycle takes between 90 minutes and two hours, and most people will spend the majority of their sleeping time in stage one, stage two, and REM sleep.
Understanding Sleep Deprivation
How much sleep a person needs can vary based on age, health status, and other factors. Unfortunately, we are not always guaranteed a full night of sleep. Age and certain health problems can interfere with your ability to fall asleep, stay asleep, or get the undisturbed sleep you need.
When you regularly get too little sleep, you can become sleep-deprived. We do not adapt to sleep deprivation but instead develop a “sleep debt.” Just one sleepless night can leave you feeling drowsy and unable to focus during the day. When you consistently go without sleep, you might find yourself falling asleep unexpectedly. Sleep-deprived drivers are more likely to experience a vehicle crash.
Inadequate sleep does not just leave you feeling groggy. It can affect every part of your body, increasing your risk of depression, high blood pressure, obesity, diabetes, heart attack, and stroke. High-quality sleep is essential for good health and proper function, and if you fail to get it, your body and mind will struggle until your sleep debt is paid.
Dealing with Sleep Disorders
Millions of people around the world suffer from disordered sleep. About a third of adults worldwide experience periodic wakefulness while 10 percent suffer from chronic insomnia. Obstructive sleep apnea or OSA is another common issue that affects between 9 and 31 percent of adults. Both of these disorders can prevent you from getting enough high-quality sleep to support healthy function, but a lesser-known sleep disorder, sleep paralysis can create anxiety surrounding sleep and make it hard for you to relax enough to go to sleep. About 7 percent of the general population experiences paralysis during sleep, but that number quadruples in those who suffer from panic disorder.
If you have a sleep disorder, you might not cycle through the sleep stages properly or have a hard time getting the sleep you need. Your sleep debt will increase as your function and health are put at risk. Proper diagnosis and management of disorders of sleep can help people get the sleep they need and protect their health.
Insomnia
Virtually all of us will experience a bout of sleeplessness at some point. This sleep disorder is often associated with stress, anxiety, a change in diet, or even jet lag. While a day or a couple of days might not cause serious issues, an ongoing lack of sleep can increase your sleep debt and threaten your wellbeing.
Insomniacs often have a difficult time falling asleep, staying asleep, or sleeping without interruption. You might be at a higher risk of developing this sleep disorder if you:
- Are older
- Have a family history of the disorder
- Are female
- Experience excessive stress
- Travel to different time zones frequently
- Engage in shift work
- Have an irregular sleep schedule
- Are sedentary or inactive during the day
- Watch TV or use electronic devices near bedtime
- Use caffeine, nicotine, alcohol, or other substances
Addressing the lifestyle factors that may be aggravating or causing your poor sleep can make a big difference. This might mean reducing caffeine consumption before bedtime or improving stress management.
Good sleep hygiene can go a long way towards counteracting poor sleep, which is why conservative lifestyle changes are typically the first-line treatment for insomniacs. If you are struggling to sleep, skip the daytime naps or limit them to 30 minutes or less. Exercise regularly during the day, and eat a balanced diet. Avoid watching TV or using devices in your bedroom, and keep that space dedicated to healthful sleep habits.
A bedtime routine can also be beneficial and can help you unwind before you sleep. Try reading a relaxing book, taking a warm bath, or drinking a cup of chamomile tea.
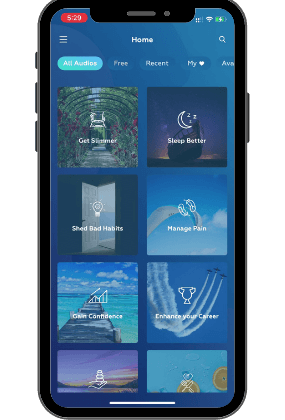
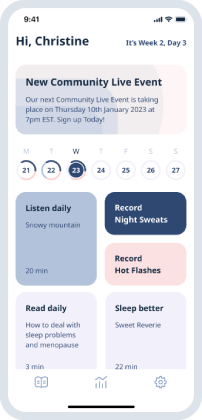
If your sleep disruptions continue despite lifestyle changes, it may be time to consider other therapies, such as meditation, counseling, massage therapy, or hypnotherapy. These therapies are designed to calm and relax you, boost your stress management skills, and help you develop a healthier mindset surrounding sleep.

Sleep Apnea
OSA is the most common type of apnea. In people with OSA, the windpipe collapses during sleep, briefly obstructing the airway. When the brain senses oxygen levels declining, it wakes up so that you can clear your airway. People with OSA might wake up a few to dozens of times a night.
Several factors can cause or contribute to OSA, including excess weight, lost muscle tone, age, certain medications, and health issues. You might also be at a higher risk of OSA if you smoke or use alcohol before bedtime.
Symptoms of OSA can include:
- Loud or chronic snoring
- Daytime sleepiness and difficulty concentrating
- Abruptly awakening with a sensation of gasping or choking
- Waking with a dry mouth, sore throat, or headache
- Depression or irritability
Others may also observe pauses in breathing in people with OSA.
Because lifestyle factors can contribute heavily to OSA, addressing them can help improve your breathing at night. Common changes can include:
- Regular exercise
- Weight loss for overweight people
- Reduced alcohol consumption, especially before bedtime
- Smoking cessation
- A change in sleeping position
If addressing lifestyle factors does not provide the necessary relief, your doctor may recommend other therapies, including continuous positive airway pressure or CPAP, which can help maintain an open airway during sleep, or oral appliances, which adjust the jaw’s positioning to widen the airway.
Sleep Paralysis
This sleep disorder might not be life-threatening as OSA can be, but it can trigger significant fear and anxiety in those who suffer from it. When you experience paralysis during sleep, you may be unable to move when you first fall asleep or awaken. You will be able to hear, see, and feel, but you may experience a heavy sensation or pressure. You might also have visual, auditory, or sensory hallucinations, which can induce feelings of terror or panic.
While episodes of paralysis are typically brief, lasting anywhere from a few seconds to a few minutes, the fear and anxiety they engender can stay with you long after the moment has passed.
This disorder occurs as a result of your body and brain getting out of sync during the sleep cycles. Your mind wakes up, but your body is still asleep.
You might be more at risk of paralysis during sleep if you have:
- Narcolepsy
- An irregular sleeping schedule
- A family history of the disorder
- Migraines
- Clinical depression or anxiety
- High blood pressure
- OSA
There are no formal treatments, but lifestyle changes can reduce your risk of suffering an episode. Maintaining a regular sleep schedule, managing stress, and maintaining good sleep hygiene can all be beneficial.
You might also wish to keep your bedroom cool and quiet, wear comfortable sleepwear, and use light therapy to promote healthier sleep-wake cycles. As with other sleeping disorders, you might find relief by eating lightly before bedtime, avoiding alcohol or caffeine too close to bedtime, exercising regularly, and developing a calming bedtime routine.
Restorative sleep is essential for good health, but disordered sleep can keep you from getting the rest you need. Taking steps to promote healthier day-to-day habits, especially surrounding your sleep routine, can play a role in your recovery. Start today by taking the UpNow Sleep Quiz and assess the quality of your sleep hygiene.
UpNow Health only uses high-quality sources, including peer-reviewed articles, to support the facts within our articles. All our articles are reviewed by experts to ensure that our content is accurate, helpful, and trustworthy.
1. Purves D, Augustine GJ, Fitzpatrick D, et al., editors. Neuroscience. 2nd edition. Sunderland (MA): Sinauer Associates; 2001. Stages of Sleep. Available from: https://www.ncbi.nlm.nih.gov/books/NBK10996/
2. Colten, H. R., & Altevogt, B. M. (2006). Extent and health consequences of chronic sleep loss and sleep disorders. Nih.gov; National Academies Press (US). https://www.ncbi.nlm.nih.gov/books/NBK19961/
3. Brown WD . Lee-Chiong T. Insomnia: prevalence and daytime consequences , Sleep: A Comprehensive Handbook, 2006 Hoboken, NJ, John Wiley and Sons (pg. 93-98) Google Scholar
4. Ferrie, J. E., Kumari, M., Salo, P., Singh-Manoux, A., & Kivimaki, M. (2011). Sleep epidemiology–a rapidly growing field. International Journal of Epidemiology, 40(6), 1431–1437. https://doi.org/10.1093/ije/dyr203
5. NHS Choices. (2018, May 30). Sleep and Tiredness. NHS. https://www.nhs.uk/live-well/sleep-and-tiredness/why-lack-of-sleep-is-bad-for-your-health/
6. Sleep apnea. National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health-topics/sleep-apnea. Accessed March 15, 2021.
7. Chang, H-P, Chen, Y-F, Du, J-K. Obstructive sleep apnea treatment in adults. Kaohsiung J Med Sci. 2020; 36: 7– 12. https://doi.org/10.1002/kjm2.12130
8. What is obstructive sleep apnea? American Thoracic Society. https://www.thoracic.org/search.php?cx=007982365765420951334%3A7u3jtkdzuqu&cof=FORID%3A10&ie=UTF-8&q=sleep+apnea&sa=&siteurl=www.thoracic.org%2F&ref=www.thoracic.org%2Fsearch.php%3Fcx%3D007982365765420951334%253A7u3jtkdzuqu%26cof%3DFORID%253A10%26ie%3DUTF-8%26q%3Dsleep%2Bapnea%26sa%3D%26siteurl%3Dwww.thoracic.org%252F%26ref%3Dmedlineplus.gov%252F%26ss%3D2396j659698j11&ss=1839j485003j11
9. Strausz, S., Kiiskinen, T., Broberg, M., Ruotsalainen, S., Koskela, J., Bachour, A., FinnGen, Palotie, A., Palotie, T., Ripatti, S., & Ollila, H. M. (2021). Sleep apnoea is a risk factor for severe COVID-19. BMJ open respiratory research, 8(1), e000845. https://doi.org/10.1136/bmjresp-2020-000845
10. Hooper R. G. (2020). CPAP Therapeutic Options for Obstructive Sleep Apnea. Pragmatic and observational research, 11, 67–76. https://doi.org/10.2147/POR.S258632
11. Sleep deprived people more likely to have car crashes. (2018). ScienceDaily. https://www.sciencedaily.com/releases/2018/09/180918082041.htm
12. Sleep Disorders. (2018). Medlineplus.gov; National Library of Medicine. https://medlineplus.gov/sleepdisorders.html
13. What is sleep paralysis? American Academy of Sleep Medicine. Sleep Education. https://sleepeducation.org/sleep-disorders/
14. What is sleep paralysis? American Academy of Sleep Medicine. Sleep Education. https://sleepeducation.org/sleep-disorders/sleep-paralysis/
15. Sleep paralysis. (n.d.). Stanfordhealthcare.org. https://stanfordhealthcare.org/medical-conditions/sleep/nighttime-sleep-behaviors/sleep-paralysis.html
16. NHS. Sleep Paralysis. https://www.nhs.uk/conditions/sleep-paralysis/
17. Denis, D., French, C. C., Rowe, R., Zavos, H. M., Nolan, P. M., Parsons, M. J., & Gregory, A. M. (2015). A twin and molecular genetics study of sleep paralysis and associated factors. Journal of sleep research, 24(4), 438–446. https://doi.org/10.1111/jsr.12282
18. Olunu, E., Kimo, R., Onigbinde, E. O., Akpanobong, M. U., Enang, I. E., Osanakpo, M., Monday, I. T., Otohinoyi, D. A., & John Fakoya, A. O. (2018). Sleep Paralysis, a Medical Condition with a Diverse Cultural Interpretation. International journal of applied & basic medical research, 8(3), 137–142. https://doi.org/10.4103/ijabmr.IJABMR_19_18
19. American Sleep Association. Sleep Paralysis: Causes, Symptoms and Treatments. https://www.sleepassociation.org/sleep-disorders/more-sleep-disorders/sleep-paralysis/